
Fertility treatment options are used for a number of reasons, including infertility, a family history of a genetic condition, and to achieve pregnancy by members of the LGBTQ community. While the impetus for seeking treatment may differ, the procedure options remain the same.
Treatments include a range of options from fertility preservation; sperm, egg and embryo donation; gestational surrogacy; intrauterine insemination; and in vitro fertilization.
For the sake of simplicity, this article will focus on practices available within the United States.
Fertility Preservation Options
Hormone therapy, such as feminizing or masculizing hormones, is an option some transgender individuals may pursue throughout their lifetime. According to the Standards of Care for the Health of Transexual, Transgender, and Gender-Nonconforming People published by The World Professional Association for Transgender Health, hormone therapy can limit fertility. While some transgender patients who choose to use this option may be able to conceive on their own by temporarily postponing hormone therapy, some may need to use one or more of the options described below.
For transgender men, two fertility preservation options (FPOs) are oocyte cryopreservation and embryo cryopreservation. The former is a process that freezes and stores unfertilized eggs for later use, while the latter is a process that freezes and stores fertilized eggs for later use. For transgender women, FPOs include sperm cryopreservation or surgical sperm extraction.
Transgender individuals who are considering hormone therapy and/or surgical options that modify reproductive organs should consider their fertility desires and have open discussions about their reproductive options with their health care team.
Gamete Donors
Sperm donor
Individuals in the LGBTQ community may elect to use a sperm donor. There are two main options for selecting a sperm donor: known or anonymous/non-identified donor. For patients who prefer to use semen from a known donor, sperm analysis is relatively inexpensive and non-invasive. Sample collection may be performed at either a laboratory, a physician’s office or, in some cases, the privacy of one’s home. If using an anonymous donor, the fertility clinic you elect to work with will assist you by providing information on available donor sperm banks and will discuss types of vials of sperm available and how many are recommended.
Egg donor
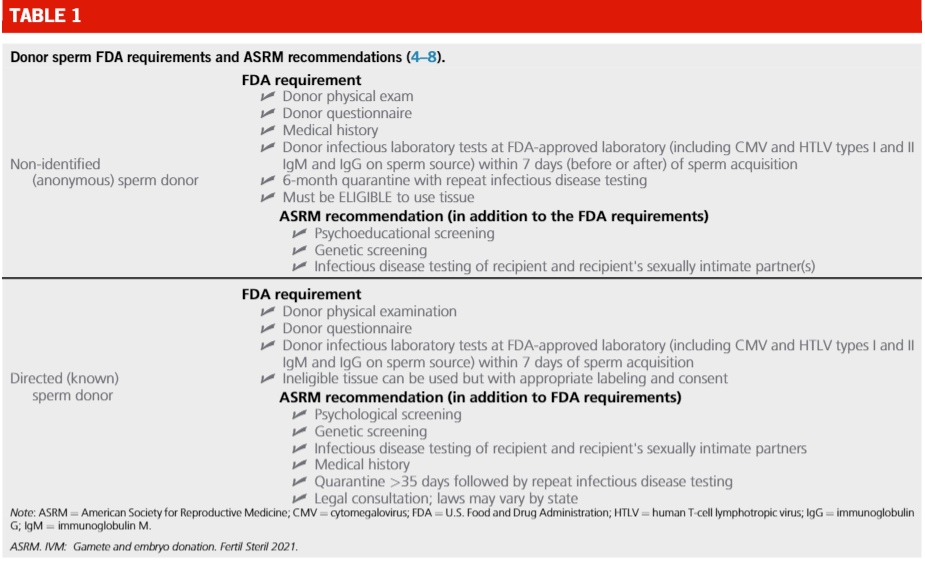
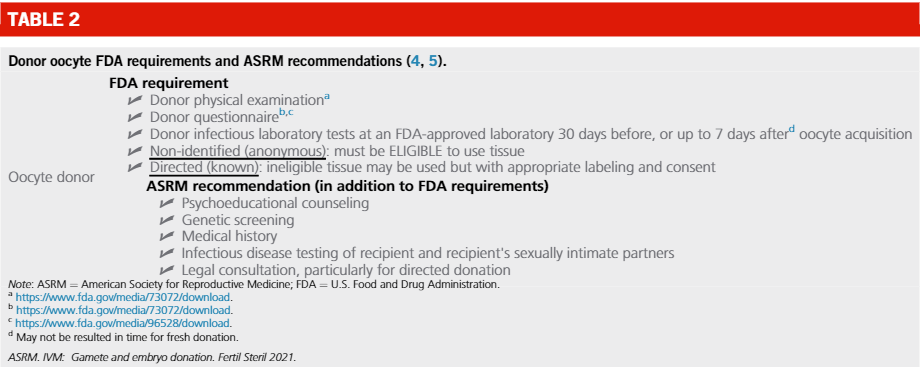
Other individuals in the LGBTQ community may utilize the option of a known or anonymous/non-identified egg donor. In either case, if a donor egg is used and is not from a surrogate who will be the gestational carrier, the collection of the oocyte is done in a clinic. While there are no universally accepted standards for gamete and embryo donors and recipients, and while minimum screening and testing requirements differ from state to state, guidance and recommendations do exist from professional societies such as the Food and Drug Administration, Centers for Disease Control and Prevention and American Society of Reproductive Medicine. In the latest released document, the two following tables detail what is required versus what is recommended.
Assisted Reproductive Technology Options
Whether the patient is single or the couple is two women, two men, transgender or any combination thereof, two common fertility procedures to achieve a pregnancy for LGBTQ families are intrauterine insemination (IUI) and in vitro insemination (IVF). In addition, couples or individuals who do not have a uterus will require the use of a surrogate to carry the pregnancy. Like gamete donors, gestational carriers must meet stringent criteria that may include a review of their medical history and various medical evaluations. There are important laws to consider when using a gestational carrier. Since parental rights and obligations can vary from state to state, we recommend patients consult with an experienced attorney that specializes in third-party reproduction.
IUI
While at-home insemination is an option with a known donor and has the benefit of being less expensive, it is not for everyone. It has a lower success rate, requires at-home tracking of one’s cycle, and may be unsuitable for those with underlying fertility issues such as endometriosis or polycystic ovarian syndrome. Most conceptions with either an anonymous or known donor are performed through a fertility clinic, often with the use of medications to stimulate the ovary and promote ovulation. Alternatively, insemination can be timed during a woman’s natural ovulation cycle. Near the time of ovulation, sperm is placed directly into the uterine cavity through a small catheter.
IVF
IVF involves fertilization of an egg outside the body. Sperm is placed directly with the retrieved eggs in the laboratory to create embryos, which can then be transferred to the uterus or cryopreserved for future use. As circumstances differ, any one scenario below may or may not be right for any given patient. For lesbian couples or couples without male sex reproductive organs, potential options may include:
- IVF, using the eggs of one partner and fertilized by donor sperm, the embryo is implanted into the other partner. This is also known as co-IVF or reciprocal IVF. Many lesbian couples choose this shared path, switching who provides the egg and who is the gestational carrier in a subsequent pregnancy.
- IVF, using the eggs of one partner and fertilized by donor sperm, the embryo is implanted into a surrogate.
- IVF, using donor eggs and donor sperm, the embryo is implanted into one partner.
- IVF, using donor eggs and donor sperm, the embryo is implanted into a surrogate.
- IVF, using eggs from both partners and donor sperm, the embryo is implanted into one partner.
- IVF, using eggs from both partners and donor sperm, the embryos are implanted into both partners.
- IUI, using donor sperm and inseminating into one partner’s uterus
For gay couples or couples without female sex reproductive organs, potential options may include:
- IVF, using donor eggs and sperm from one or both partners, the embryo is implanted into a surrogate. While it’s only possible to use the sperm from one man to fertilize any given egg, some gay couples choose to do split insemination, in which half of the eggs are put with one man’s sperm and the other half are put with the other man’s sperm.
- IVF, using donor eggs and donor sperm, the embryo is implanted into a surrogate.
- The egg from a surrogate is fertilized by a partner or donor sperm through IUI. Termed traditional surrogacy, this is a less expensive option in which the surrogate is the baby’s genetic mother.
Genetic Testing Options
In each pregnancy, there is a 3-4 percent chance of a genetic condition, chromosome abnormality, birth defect, or intellectual disability, many of which are not detectable through any diagnostic or screening technique. As stated above, there are no universally accepted standards for gamete and embryo donors and recipients. This also applies to the topic of genetic carrier screening of donors for heritable diseases and family history screening for genetic conditions, congenital anomalies, multifactorial conditions and chromosome conditions. However, there are preconception, preimplantation and prenatal genetic testing options available to assess the risk for your pregnancy to be affected with certain genetic conditions and chromosome conditions.
Genetic conditions
Prior to starting fertility treatments, carrier screening is recommended for parents-to-be. Carrier screening can be limited to single conditions, like cystic fibrosis, spinal muscular atrophy or Fragile X syndrome, or can be expanded to include hundreds of conditions. Although carrier testing can identify individuals at risk to have a child with a genetic disease, which may lead to additional testing, it is not an exhaustive screening with respect to the risk for all possible genetic conditions, chromosome abnormalities, birth defects or intellectual disabilities.
The typical number of chromosomes is 46. Those assigned male at birth typically have an X chromosome and a Y chromosome, while those assigned female at birth typically have two X chromosomes. Carrier screening panels screen for conditions that follow two forms of inheritance: autosomal recessive and X-linked. Those assigned female at birth are screened for both, while those assigned male at birth are only screened for autosomal recessive conditions. This is because someone with two X chromosomes can carry a variant on one of their X chromosomes and not show signs or symptoms of a condition, but have a 50% chance to pass the genetic variant to a son who would then be affected. As such, carrier screening for X-linked conditions, in addition to autosomal recessive conditions, is recommended for anyone assigned female at birth.
This testing can be done at any time, but is recommended prior to conception for two reasons:
- If you are determined to be a carrier of an autosomal recessive genetic condition, it is recommended that your donor or reproductive partner be screened for the same condition to accurately assess the risk of having an affected child.
- If you are identified to be at an increased risk of having an affected child with either an autosomal recessive or X-linked condition, additional testing may be available to reduce that risk. Early screening allows for additional time for discussions and planning.
Chromosome conditions
As previously stated, the typical number of chromosomes is 46. Assessing if the correct number of chromosomes are present can be performed through genetic screening and/or diagnostic genetic testing.
Preimplantation genetic testing for aneuploidy (PGT-A) is the only option that can be done prior to pregnancy. Though termed “testing,” this is not a diagnostic test, but rather is a screening test. It is important to know the difference between the two. (PGT-A) is typically performed on day 5, where the embryo has 100-200 cells. Routine day 5 biopsies typically contain between 5–10 cells. Blastocyst biopsies are taken from the trophectoderm (TE), which goes on to form the placenta; the inner cell mass (ICM) goes on to form the fetus. Of note, PGT-A cannot be performed with IUI or traditional surrogacy but can be performed with IVF.
Numerous prenatal genetic screening and testing options, including non-invasive prenatal testing, chorionic villi sampling, amniocentesis and a detailed anatomy scan, are also available.
In Summary
Any fertility process is deeply personal and best handled with the help of a team of medical professionals committed to your care who are willing to answer all of your questions and guide parents-to-be on their way to becoming a family.
Whether you are gay, bisexual, trans or something else, if you want to have a baby, there are numerous fertility treatments options available to you.

